General Evaluation and Breast Evaluation
 As with any surgical procedure, a medical history and physical exam should be performed when considering breast reduction or breast lift, especially for patients that do not receive regular medical care. During the history, information regarding the patient’s general health is assessed. This is especially true for older patients who are more likely to have general health issues (heart, blood pressure) which may complicate the procedure than younger patients. The patient’s symptoms are reviewed (as noted in a previous section) and they fit a typical pattern in most patients. Any psychological or social problems are also reviewed. The patient’s family history related to breast cancer should also be explored. The importance of the patient’s family history of breast cancer becomes more important with advancing age (although it is important at any age) because the incidence of breast cancer increases as age increases. A strong family history of breast cancer should always be considered when planning any type of breast surgery. A family history of breast cancer is a risk for developing breast cancer. In some circumstances, a strong family history of breast cancer may completely change the surgical plan. Some patients have an inherited genetic tendency to develop breast cancer. A percentage of patients have a known genetic trait (BrCa) which increases the risk of breast cancer. If this is suspected, then a consultation with qualified specialist is obtained to complete genetic testing. Fortunately, the minority of patients (based on current data) that develop breast cancer are a result of an identified genetic trait.
As with any surgical procedure, a medical history and physical exam should be performed when considering breast reduction or breast lift, especially for patients that do not receive regular medical care. During the history, information regarding the patient’s general health is assessed. This is especially true for older patients who are more likely to have general health issues (heart, blood pressure) which may complicate the procedure than younger patients. The patient’s symptoms are reviewed (as noted in a previous section) and they fit a typical pattern in most patients. Any psychological or social problems are also reviewed. The patient’s family history related to breast cancer should also be explored. The importance of the patient’s family history of breast cancer becomes more important with advancing age (although it is important at any age) because the incidence of breast cancer increases as age increases. A strong family history of breast cancer should always be considered when planning any type of breast surgery. A family history of breast cancer is a risk for developing breast cancer. In some circumstances, a strong family history of breast cancer may completely change the surgical plan. Some patients have an inherited genetic tendency to develop breast cancer. A percentage of patients have a known genetic trait (BrCa) which increases the risk of breast cancer. If this is suspected, then a consultation with qualified specialist is obtained to complete genetic testing. Fortunately, the minority of patients (based on current data) that develop breast cancer are a result of an identified genetic trait.
The patient’s general natural scarring tendency is assessed. Some idea of the patients natural scar forming tendency can be determined from the patients history and physical exam. The best predictor of the next scar is the last scar. Because breast reduction and breast lift require relatively long incisions (as compared to augmentation mammplasty), the patients natural scar forming ability is important. The patient’s history of tobacco use and secondary tobacco exposure are explored. Breast reduction and breast lift procedures involve the use of “flaps” which can be adversely affected by tobacco exposure. Tobacco use can decrease the circulation in the “flaps” which can cause tissue loss and delayed wound healing. This is more critical in breast reduction and breast lift than breast augmentation. Secondary smoke exposure (breathing smoke from another persons cigarettes) also increases the risk of other wound problems, so this should be avoided as well. It is advisable that patients stop smoking for a period of time before and after breast reduction or breast lift. Many surgeons require that patients avoid primary and secondary exposure to tobacco be avoided in the peri-operative period. Even if a patient stops smoking before and after surgery there is still some increased risk for healing problems (infection, delayed wound healing, wound separation, tissue loss) in chronic smokers. Any other health issues, such as high blood pressure that may adversely affect the procedure or exposure to anesthesia, are also explored.
In addition to the general screening exam, the breasts are also examined before surgery. The size and shape of the breasts are assessed. General breast symmetry is assessed, which includes nipple-areolar symmetry, size symmetry, shape symmetry, chest wall symmetry, and breast position symmetry. Objective breast measurements are also helpful in surgical planning. The degree of ptosis is measured (the distance of the nipple-areolar complex from the sternal notch) which helps plan the breast reduction or breast lift surgery. The integrity of the skin, breast gland, and breast ligaments are assessed. Any other issues related to the breasts are also assessed including bra strap grooving, rashes, back pain, neck pain, shoulder pain, arm and hand pain, arm and hand numbness, breast pain, muscle hypertrophy (overgrowth), skin hyperpigmentation (dark skin), and any limitations of physical activity.
Breast imaging (x-rays) and other breast screening studies (ultrasound and MRI) may be performed in some patients. There are no hard and fast rules for breast (cancer) screening, but the American Cancer Society guidelines are a reasonable place to start when determining the need for screening. Breast cancer screening techniques are not perfect, but are better than no screening at all. In most circumstances, routine screening for breast cancer is best performed by the patient’s primary care physician. Screening for breast cancer before a breast reduction or breast lift is sometimes ordered by the Plastic surgeon when, for whatever reason, the patient has not had screening ordered by the primary care physician. If the patient has already had breast screening by their primary care physician then further screening may not be necessary. In the case of the Plastic surgeon, the screening falls into the category of “pre-operative workup”. After the procedure, screening should be resumed by the primary care physician as a part of routine care. All patients presenting for breast reduction or breast lift do not necessarily need breast imaging. If the patient falls into the general category of recommendation according to the American Cancer Society then breast cancer screening is considered. The general guidelines for breast cancer screening can be found on the American Cancer Society website.
The breast reduction, and to a lesser degree, the breast lift procedure, is thought to reduce the incidence of breast cancer. While the breast reduction and the breast lift procedures may decrease the incidence of breast cancer, this is not a reason to get one of these procedures. Rather, this is a beneficial side effect when the procedure is performed. From the aforementioned conclusion, one can also infer that breast reduction and breast lift do not cause breast cancer. For patients that have a high risk of breast cancer a more complete removal of breast tissue may be desired, which may require a subsequent reconstructive procedure.
The Consultation Process
A consultation is provided (at no cost) to the patient before breast reduction or breast lift procedures. During that consultation the informed consent process is completed. The informed consent process reviews information related to the breast reduction and breast lift so that the patient can make an informed decision about the procedures. The patient also has the opportunity to ask questions about the procedure and request further information if so desired. If the patient wishes to come back for additional consultation (at no cost) this is also completed. Family members are welcome to attend the consultation(s) and ask questions if (and only if) the patient so desires.
Breast Reduction Volumes
Breast reduction has been divided into several categories subjectively based on the amount of tissue removed during the procedure. These values are completely subjective, meaning that other methods of categorizing breast reduction weights are also acceptable. The table below subjectively divides breast reduction into separate categories based on the amount of tissue (weight in grams) removed during the procedure. The amount of breast tissue (by weight) to be removed can be estimated before surgery, but predicting the exact quantity (by weight) is extremely difficult or impossible.
| Category of Breast Reduction |
Grams of Breast Tissue Removed |
| Small |
< 200 grams per side |
| Medium |
200 to 500 grams per side |
| Large |
500 to 1800 grams per side |
| Gigantic |
> 1800 grams per side |
Formulas have been used to help predict how much breast tissue will be removed during the breast reduction procedure, but these formulas are useful only as a rough estimate. The patient’s desire for a specific final breast size is important to consider during the pre-operative planning, but it is also important for the patient to understand that an exact bra “cup size” cannot be accurately predicted. Because there is no consistency between bra manufacturers regarding the volume of the breast volume as related to “cup size”, a specific “cup size” can only be used as a very rough estimate during pre-operative planning.
Breast Shape after Breast Reduction and Breast Lift
The breast shape naturally changes as a patient ages. If any significant breast volume (weight) exists, there is usually some ptosis (sagging) to go along with it. Breast ptosis (sagging) is defined by the relationship of the nipple-areolar complex to the sternal notch (see the chart and images in the breast augmentation mammaplasty section). The most mild form of breast ptosis (sagging) is termed pseudoptosis (false sagging). Psuedoptosis (false sagging) is more of a change in the shape of the breast than actual sagging of the breast. The most severe form of breast ptosis (sagging) is termed grade III. In grade III ptosis, the nipple is below the infra-mammary fold and is also in the lowest portion of the breast (below the breast mound). Grade I breast ptosis and Grade II breast ptosis fall between pseudoptosis and grade III breast ptosis.
The goal after breast reduction or breast lift is to achieve a breast shape of a mature person. This would include a sternal notch to nipple-areolar distance of 19 to 23 centimeters and a slightly pendulous shape. All breasts of any size have some degree of ptosis (sagging), and this is the most natural appearance. There is generally more fullness in the lower outer quadrant and the lower inner quadrant with less fullness in the upper half of the breast in the mature female breast. A perfect conical breast in the mature female patient does not appear as natural, and is not the goal with any breast procedure, including breast augmentation, breast reduction, or breast lift. A perfect conical breast is very difficult or impossible to achieve in long term results with any breast procedure. It is also important to note that shaping a very large breast during breast reduction is much more challenging than shaping a slightly large breast for a number of reasons.
Breast Reduction and Breast Lift Procedures
There are many different procedures that are described to achieve the breast reduction or the breast lift, and they all have advantages and disadvantages. As with breast augmentation, the patient’s specific anatomy determines, in part, which specific procedure is recommended to the patient. As with any cosmetic procedure, no single procedure is a perfect match for every patient’s specific anatomy. Not only is the type of procedure varied from patient to patient (depending upon anatomy and goals), variation within each procedure is also commonly utilized. In other words, no two procedures are exactly alike, but rather are customized for each patient. Because breast shape is so widely varied, the technique chosen is varied to meet the patients specific anatomy. While there are many techniques described, the surgical procedures described below describe the general range of procedures that are commonly performed to achieve breast reduction and breast lift. As with all Plastic surgery procedures, selection of the optimal procedure for each individual patient is key.
The Peri-areolar Breast Reduction and Breast Lift
The peri-areolar breast reduction and breast lift procedure, also called the “donut” breast lift procedure, can be used for very small breast reductions or minimal breast lifts. The incisions for the peri-areolar breast reduction and breast lift are at the border of the areola and may also include a very short vertical incision below the areola as well (see vertical breast reduction and breast lift in subsequent section). The peri-areolar breast reduction allows a minimal amount of breast reduction and/or lifting. The tissue that is removed is above, below, and on the sides of the nipple-areolar complex. Breast tissue is removed and rearranged through the periareolar incision which avoids a large vertical and horizontal incision. This procedure can be useful when a very small breast reduction is desired and the patient also has an areolar diameter than is larger than normal (greater than 4.5 centimeters in diameter).
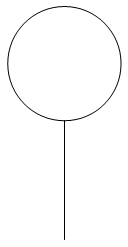
Because skin and/or areolar tissue is removed with this technique, a normal sized areolar complex (3.5 to 4.5 centimeters) can be achieved in the situation when the areolar complex is too large (a maximum diameter of over 4.5 centimeters). In this case, the areola is partially excised and the surrounding breast skin is advanced into that space. The peri-areolar breast reduction and breast lift may be more challenging in patients with a smaller than normal areola. The peri-areolar breast reduction and breast lift can also be useful in patients with a “tubular breast deformity”. In this circumstance, the breast tissue is herniated into the nipple-areolar complex causing excessive protrusion. A primary problem encountered with the peri-areolar procedures (besides being limited to very small breast reductions and breast lifts) is poor (unfavorable) scarring. The poor (unfavorable) scarring that is sometimes observed results from two factors. First, the skin edge on the outer part of the incision is longer than the edge of the areola which is on the inner part of the incision. As a result, there may some wrinkling or irregularities of the final scar as these two areas are repaired (see the diagram below showing the mismatch of wound edges). Second, after the skin and areola are sutured, if there is an excess amount of tension on the repaired area, the scar has a tendency to widen over time. One of the goals of any cosmetic surgery is to achieve a linear (narrow) healed scar as opposed to a wide scar. When there is excess tension within a healing (skin) scar anywhere in the body the final scar is widened. Because living tissue is dynamic (and as a basic characteristic, living things respond to their environment), it will react to outside stress or tension which results during wound closure.
-

-
Wound edges before closure
-
-
Wound edges after closure
Excess tension may also expand the areola to the degree that it is beyond the width of the normal diameter (resulting in recurrence of the original problem). The end result may be a very large areola surrounded by a wide scar. In some circumstances placement of synthetic (man-made) mesh has been placed in the wound to assist in support and prevent scar widening and areola widening. While synthetic mesh may help provide support and prevent scar widening and areola widening to some degree, it may also cause long term problems such as infection, distortion, and interference with breast cancer screening. Because the mesh is placed inside the breast parenchyma (tissue), mammograms may become more technically difficult to obtain and interpret. Another technique to prevent scar widening is placement of a “permanent” suture in the wound. This technique is called the “purse string suture”, which is a continuous suture around the nipple-areolar complex that will theoretically help hold the skin centrally and prevent scar widening and areola widening. In summary, if excess tension is placed on the nipple-areolar complex with the closure of surgical wounds, the end result may be a very wide nipple-areolar complex (too wide, > 4.5 centimeters) that is surrounded by a very wide irregular scar. The key is to minimize wound tension for optimal scarring, good shape, and minimal scar burden. In addition to those potential problems, the mesh and sutures at the breast may be palpable (can feel the material through the skin), which is obviously undesirable.
Another potential problem with the peri-areolar procedure is flattening of the breast, especially the anterior (front part around the nipple areolar complex) aspect of the breast. In this circumstance, the central portion of the breast surrounding the nipple areolar complex may appear retracted. This can be a result of the “purse string” compression of the anterior breast tissue, and the flattening would give the breast an unnatural appearance. In this circumstance, there would be a decrease in breast projection, contrary to one of the primary goals of the procedure.
Vertical breast reduction and breast lift
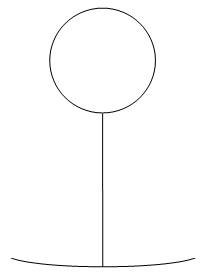
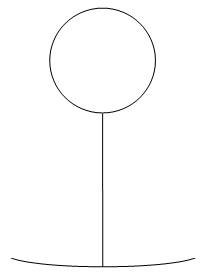
The vertical breast reduction and breast lift is well suited for patients that are of normal body weight and have a moderate amount of excess tissue or sagging. This procedure has similarities to the peri-areolar breast reduction and breast lift except there is an additional vertical scar below the nipple-areolar complex. This scar extends to, and preferably ends above, the inframammary fold. This procedure has been referred to as the “lolly pop” procedure due to the shape of the scar (see diagram below).
Shape of scar for vertical reduction mammaplasty and breast lift
The vertical breast reduction and mastopexy removes tissue from the lower central aspect of the breast, and the nipple-areolar complex is supported (vascular supply) by a developed pedicle in the superior, medial, or lateral aspect of the breast. The vertical breast reduction is estimated to potentially reduce up to 50% of the existing breast volume. The ideal patient for this type of procedure is one with (approximately) normal weight, a very well perfused (good circulation) breast gland, good skin integrity (elasticity), a moderate amount of excess tissue, and a small or moderate degree of ptosis (sagging). The obvious advantage of the vertical breast reduction and vertical mastopexy is the limited length of skin scars (no horizontal scar) when compared to the Wise pattern breast reduction (see subsequent section on that topic).
Another advantage of the vertical breast reduction and the vertical breast lift is the ability to achieve excellent breast projection. This is a result of the dynamics of the flaps that are advanced. A disadvantage of the vertical breast reduction and the vertical breast lift is the challenge of treating the patients with severe breast ptosis (sagging), extremely large amounts of excess breast tissue, and patients that are overweight. The overweight patient is especially challenging because typically there is excess tissue (breast tissue and fat) in the lateral aspects of the trunk (under the arms, termed axillary breast tissue). Another disadvantage is the potential for tissue redundancy and irregular folds in the area of the infra-mammary fold. The likelihood of tissue redundancy and irregular fold increases as the size of the breast increases and the ptosis (sagging) increases. The vertical breast reduction and the vertical breast lift can be modified to reduce these problems with a short infra-mammary incision which allows management of the redundant tissue in the central infra-mammary fold area, which is very similar to the Wise pattern breast reduction or breast lift. Many variations of this additional incision have been described. Yet another potential problem is scar widening, especially in the vertical scar. If excess tension is placed on the vertical closure in an attempt to avoid a horizontal scar, this may result in a wide unsightly vertical scar.
The Wise pattern (inferior pedicle) breast reduction and breast lift
The Wise pattern breast reduction and breast lift has been described as the most commonly performed breast reduction and breast lift technique. It was described by Dr. Robert Wise in 1956 and it is the standard to which all other breast reduction techniques are compared. A multitude of variations of this technique have been described. It is also termed the inferior pedicle breast reduction or inferior pedicle breast lift technique. The inferior pedicle breast reduction or inferior pedicle breast lift techniques adds an extra horizontal scar (to the vertical breast reduction or breast lift) of varying length in the area of the infra-mammary fold. It has also been referred to as the “anchor design” due to the appearance of the final scar as the breast is viewed from the front (see diagram below).
Wise pattern (inferior pedicle) reduction mammaplasty and breast lift
The inferior pedicle breast reduction or inferior pedicle breast lift technique also supports (provides blood supply) the nipple areolar complex on a pedicle (flap). However, instead of the pedicle being in the superior (top), medial, or lateral portion of the breast as in the vertical breast reduction and the vertical breast lift, in this procedure the pedicle is in the inferior aspect (bottom) of the breast. The excess breast tissue is typically removed from above and on both sides (medial and lateral) of the pedicle in the inferior pedicle breast reduction or inferior pedicle breast lift technique. After the excess tissue is removed, the pedicle (flap) is advanced superiorly into the space created by the breast tissue removal. When the inferior pedicle breast lift technique is used, a minimal amount of tissue is removed before the inferior pedicle flap is advanced superiorly. In this case, the flaps (pedicles) are developed (created) primarily to facilitate tissue rearrangement. After removal of the excess tissue, the medial and lateral flaps that are developed in conjunction with the inferior pedicle are then advanced to a central point at the bottom of the inferior pedicle, which is termed the “key position”. This is observed as the intersection of the two lines composing an inverted “T” (bottom central part the anchor). One advantage of the inferior pedicle breast reduction or inferior pedicle breast lift technique is the predictability of breast shape after the flaps are approximated. It also allows exact measurements of the proposed flap dimensions, which makes planning easier and the procedure more predictable. One criticism of the inferior pedicle breast reduction or inferior pedicle breast lift technique is the tendency to “bottom out”. This means that with time there is excessive fullness which develops at the bottom of the breast. This observation is not unexpected because of the position of the inferior pedicle in the inferior aspect of the breast. This can be overcome in some patients by anticipating this post-operative change and over advancing the inferior pedicle (although in some patients this is more difficult to achieve). It can also be overcome to some degree by slightly increasing the tension (but not over tightening) the inferior aspect of the breast in the area of the vertical repair. This “over tightening” in anticipation of tissue stretch can also be done with the vertical breast reduction and the vertical breast lift. It is important when creating this extra tension in the inferior aspect of the breast that the perfusion (blood supply) to that area is not compromised. The “over tightening” may also result in widening of the vertical scar. Because “settling” of the breast which leads to more fullness inferiorly with any breast reduction or breast lift technique is expected, anticipation of those changes with time leads to modifications of the technique to minimize that problem. At the completion of the inferior pedicle breast reduction or inferior pedicle breast lift, the bottom of the breast will appear slightly flat for some time. This intentionally created flatness of the inferior aspect of the breast will round out with time as the breast “settles”. In anticipation of the breast mound changes that occur after surgery, the nipple-areolar complex may appear slightly too low immediately following surgery. As the breast settles the nipple-areolar complex will appear to migrate superiorly (towards the head) to a more anatomically correct position. In actuality, it is the breast mound that moves inferiorly that gives the nipple-areolar complex the appearance of moving superiorly. Another criticism of the Wise (inferior pedicle) technique is the addition of scar burden (addition of the horizontal scars). This additional scar is in the area of eh inframammary fold (at the bottom of the breast).
The inferior pedicle technique is very useful in patients that require large reductions, in patients that have a large degree of ptosis (sagging), and in patients that are overweight. The Wise pattern breast reduction and breast lift facilitates the adjustment of the skin envelope in a superior-inferior direction (from the head to the toe) and in a medial-lateral direction (middle to the side). The included horizontal scar facilitates the removal of excess breast tissue, fat, and skin, in the medial and lateral breast in this group of patients, and allows the adjustment of the skin envelope in two dimensions (as compared to the vertical breast reduction and breast lift which is mostly adjusted in one dimension, medial and lateral). In addition to scar length, the disadvantage of the additional horizontal scar used in the the inferior technique, is that it has a tendency to be less favorable (worse appearance) than the vertical and peri-areolar scars.
While the position and orientation of this scar (horizontal and at the inferior aspect of the breast) may distract from its final appearance, there are two other factors that are important to consider. One is the patients natural scar forming tendency. As previously noted, the increased tension of the wound (skin closure) can result in spreading or widening of the healed scar. The final tension of the wound can be controlled to some degree by the surgical technique. Another factor is the patient’s natural tendency to form scars. The natural or innate scar forming tendency cannot be changed by the surgeon. If the patient is a “good scar former” then the breast scars are more likely to be aesthetically favorable. Conversely, if the patient is a “bad scar former” then the breast scars are more likely to be aesthetically unfavorable. In addition to modifying the surgical technique to minimize the final scar (by reducing wound tension), there are other modalities that can be employed to help minimize adverse scarring. One therapy is the injection of a very weak steroid directly into the scar, which favorably modifies the scar metabolism. Another modality is to use occlusive or pressure dressings, which is also believed to favorably affect the final scar. Another treatment is the application of a compound that reduces or eliminates hyperpigmentation (scar darker than surrounding skin) in the scar. This is reviewed in more detail in a subsequent section.
The free nipple graft technique breast reduction and breast lift
The free nipple graft breast reduction technique is considered in the circumstance of gigantomastia, which means patients have more than an estimated 1800 grams of tissue (per side) to remove and usually also have severe ptosis (sagging). This procedure is considered in patients with extremely large breasts (macromastia) since the circulation (blood supply) to the nipple-areolar complex may not be reliable after flaps are developed during the procedure. The free nipple graft procedure may also be considered in patients with poor circulation, in patients that use tobacco products, and in patients that are otherwise medically compromised (resulting in poor circulation). When the aforementioned patients undergo a breast reduction or breast lift by a more conventional technique, there is an increased likelihood that they will have some degree of tissue loss due to poor perfusion (blood supply), including loss of the nipple-areolar complex. This procedure is more accurately termed the free nipple-areolar complex graft technique, because more than just the nipple is transferred as a free graft. Because the nipple-areolar complex is transferred as a “free graft” in this circumstance, many different flap designs and skin patterns can be used to complete the procedure.
In patients with severe ptosis (sagging), the breast may be flat in the pre-operative state, and measures are taken to improve the projection of the breast with the free nipple-areolar complex procedure. One technique that has been described is to develop an inferior flap similar to the inferior pedicle technique, but in this circumstance, the flap (pedicle) does not support the nipple-areolar complex. In this circumstance, the pedicle is developed for the sole purpose of improving projection by providing volume in the central aspect of the breast.
There are some distinct disadvantages to the free nipple-areolar graft technique. Because the lactiferous ducts (milk ducts) are divided in order to transfer the nipple-areolar complex, the ability to breast feed is adversely affected. This procedure also interrupts the nerve supply to the nipple-areolar complex, which is likely to alter the sensation to that area after surgery. The free-nipple areolar complex graft procedure also has a tendency to de-pigment (some loss of color) the nipple-areolar graft. Due to loss of some support and scar maturation, the nipple may also lose some projection (become flatter) to some degree. When using the free nipple-areolar complex graft technique, there is also some risk of loss of that tissue, as is the case with any free grafting procedure. This is especially true in patients with poor circulation and in patients that use tobacco products. Because of the severe symptoms and psychological problems that can occur with gigantomastia, the advantages of the free nipple-areolar complex graft procedure (as compared to no treatment) outweigh the disadvantages in most of those patients. While not the most commonly performed reduction technique, the free nipple-areolar complex graft procedure does have a place in the specialty of breast reduction in selected patients. As with all surgical procedures, the indications, expected results, risks, alternatives, and complications are discussed before the procedure.
The liposuction breast reduction
Liposuction has been used for breast reduction in certain selected patients. Patients that fit the criteria for liposuction breast reduction include patients that require a limited reduction, have good to excellent skin tone, good to excellent glandular tone, and good to excellent breast ligament integrity. In the liposuction breast reduction, fat is removed from the breast though very small incisions through which a liposuction cannula is introduced. The obvious advantage of the liposuction breast reduction technique is the very small external scars as compared to the larger scars with the other techniques. The liposuction breast reduction is not as useful for removal of glandular tissue which is more resistant to removal by liposuction. Because liposuction primarily removes fat, theoretically most or all of the glandular tissue would remain in the breast after liposuction breast reduction. The result of the procedure is to reduce the contents of the “envelope” and at the same time not surgically changing the size of the envelope. Removal of breast tissue (fat) can cause an imbalance between the “skin envelope” and the total breast volume. If the “skin envelope” volume of the breast is larger than the internal structures of the breast (breast gland, breast fat, and breast ligaments) that fill it then there will obviously be “extra” (redundant) skin. Because there is no tissue rearrangement (flap development, flap advancement) or skin excision with the liposuction breast reduction technique, good to excellent elasticity of the skin is very important for a good result. In optimal candidates good elasticity of the skin will result in breast skin shrinkage after the procedure, which would theoretically lessen the amount of ptosis (sagging).
In addition to a stand alone technique, the breast liposuction technique can be used as an adjunct to the more conventional breast reduction and breast lift techniques previously described. For example, liposuction could be used in addition to the inferior pedicle breast reduction technique in the same patient. In other words, a combination of techniques are used to achieve the desired result. Because the native circulation of the breast is altered in a negative manner (decreased circulation) when flaps are developed to perform breast reduction or breast lift, extreme caution is used when liposuction is utilized in an area where flaps have been developed. This is because liposuction may further diminish the circulation of the flaps, which may result in tissue loss and other wound healing problems. A primary goal with any flap surgery (irrespective of the area of the body) is to avoid tissue loss so this is always a consideration when adding liposuction to a more conventional breast reduction or breast lift technique. Liposuction can also be used to help shape the breast during breast lift as well, albeit with caution, again, with concerns of preserving breast circulation.
Any surgical procedure, including liposuction, causes tissue trauma. Surgical trauma, however minor, always results in scarring (with fetal surgery being the possible exception). One difference between a conventional breast reduction (the previously described techniques) and a breast reduction using liposuction is the area of distribution of the internal scar. The conventional breast reduction techniques produce internal scars that are “planar”. This means that the internal scars are (for the most part) distributed in planes throughout limited areas of the breast. In distinct contrast, the internal scarring from liposuction breast reduction is not planar, but is more diffuse, and is distributed throughout the entire breast. While several studies have not shown traumatic calcification (a type of scarring that can occur in the breast after surgery) after liposuction of the breast, this possibility has been a concern for some Plastic surgeons and radiologists. The concern regarding traumatic calcifications after liposuction breast reduction is related to screening and diagnostic radiology (mammograms and other studies). Scarring inside the breast, and in particular traumatic calcifications, could potentially obscure the diagnosis of a breast cancer on mammograms and other breast screening studies. Traumatic calcifications and other scarring inside the breast certainly may make reading x-ray studies for radiologists more challenging. Diffuse scarring and oil cysts are commonly observed by radiologists many years later after patients have been treated with liposuction (for example, liposuction of the abdomen) and this could also occur in the breast after liposuction. For this reason, some Plastic surgeons are reluctant to perform liposuction on the breast proper and instead opt for more conventional techniques. Liposuction of areas outside the breast proper where breast cancers are less likely to occur may cause less chance of obscuring a breast cancer due to scarring.
Studies on the accuracy of mammograms may themselves, be less than completely accurate. This is especially true for short term studies, because the problems related to scarring versus the reading of screening and diagnostic tests may take many years to study. In other words, the problems associated with any particular treatment or therapy may not appear for many years later. Large patient groups studied over a very long period of time with randomized prospective controlled trials (RCTs) give the best data, so short term retrospective studies (studies that analyze historic cohort data ) are not believed to be as accurate or trustworthy. Scarring may also make detection of masses by physical exam more difficult.
If there is a chance a surgical specimen may contain cancer in any tissue that is removed from the body, then it should be examined grossly (with the naked eye), examined digitally (by touch), and examined under a microscope by a qualified pathologist. There are tissues that are removed from the body that arguably do not routinely need a pathologic exam (for example extracted teeth) by a qualified pathologist, but breast tissue is not one of them. Certainly, breast tissue can contain undiagnosed (undetected) cancer (could not be found on physical exam or on radiologic studies), so any breast tissue removed during surgery should always be examined by a qualified pathologist. When tissue is removed from the breast with all the previously described breast reduction and breast lift techniques, the location and orientation of the tissue is defined. In other words, the pathologist knows what part of the breast the tissue came from. In addition, the breast tissue that contained the cancer (right or left) would be known. In other words, if a cancer is incidentally discovered in a specimen from a breast reduction or a breast lift, then the approximate location in the breast will be known, and also which breast the cancer came from would be known to the pathologist. In the circumstance of liposuction breast reduction, the breast that the cancer came from (right or left) would be known, but the exact location in the breast would not be known, because the entire breast specimen would be mixed up in a single container. In this case, additional treatment (additional excision, radiation, chemotherapy, or a combination of those treatments) may be complicated because the exact location of the cancer in the breast would not be known. Liposuction primarily removes fat (as opposed to breast gland), so if a breast cancer was present, it may be left behind in the breast and not removed by the liposuction procedure. Because the breast specimen is liquified (to some degree with conventional liposuction, and more so with ultrasonic and laser liposuction), pathologic exam may be more challenging. In addition, ultrasonic and laser energy used in liposuction could conceivably liquify a breast cancer making identification more challenging for the pathologist. In this circumstance, individual cancer cells could be mixed into the entire specimen making identification of those cells very difficult or impossible with current techniques and technology. The aforementioned concerns are not reasons to avoid completely avoid liposuction of the breast, but this information should be considered in the “big picture” when choosing a breast reduction technique for a particular patient. For example, if a patient had a very strong history of breast cancer, the liposuction breast reduction procedure may not be the first choice for obvious reasons.
Another concern regarding liposuction on the breasts is related to breast tissue being exposed to potential neoplasia (cancer) inducing factors. This is especially true when considering ultrasonic liposuction and laser assisted liposuction. As with many cancer initiating entities (tobacco as a well known example), there is sometimes a very long “latent period” before the neoplastic process occurs. This means that the cancer causing effect of a particular entity may not occur until many years after the exposure. As a result, the long term effects of ultrasonic energy and laser energy when used for liposuction of the breast is not fully known at this time. Long term studies are needed to determine if liposuction, in particular ultrasonic liposuction or laser assisted liposuction, causes malignant transformation of breast tissue (glandular and ductal tissue).
Below is a summary of general guidelines for choice of breast reduction and breast lift procedures as related to specific breast anatomy and general patient habitus. There are no hard and fast rules for selection of a particular procedure, and the summary below represents only general guidelines. Augmentation mammaplasty is included because in certain selected patients with very minimal ptosis, breast implants alone will correct breast ptosis (sagging).
| Breast Anatomy |
Procedure |
| Minimal amount of ptosis |
Breast augmentation alone |
| Minimal amount of breast ptosis (sagging) and minimal amount of excess breast tissue |
Peri-areolar breast reduction or breast lift |
| Moderate amount of breast ptosis (sagging) and moderate amount of excess breast tissue |
Vertical breast reduction or breast lift |
| Moderate to large amount of breast ptosis (sagging), moderate to large amount of excess breast tissue, patient overweight |
Wise pattern (inferior) pedicle breast reduction or breast lift |
| Extreme amount of breast ptosis (sagging), extreme amount of excess breast tissue, patient overweight |
Free nipple-areolar complex breast reduction or breast lift |
| Minimal amount of breast ptosis (sagging), minimal amount of excess breast tissue, good to excellent skin elasticity |
Liposuction breast reduction |
Breast scarring after breast reduction and breast lift
In order to minimize external scarring after breast reduction and breast lift five considerations are important. The first is keeping the length of the scars at a minimum. The second is keeping the width of the scars at a minimum. The third is to maintain the optimal contour of the scars (not over or under contoured). The fourth is to maintain a normal color of the scars (so that the scar matches the adjacent skin). The fifth is to keep the scars is an optimal location, not only for optimal aesthetics, but also for optimal comfort.
Excessive tension on wounds while healing will create adverse external (skin) scarring and can also result in tissue loss. Wound tension should always be kept to a minimum (in this particular procedure). Proper flap development is very important to help minimize scar widening as the wounds heal. Proper flap development, which facilitates almost tension free advancement of the flaps creates less tension (stress) on the wound. The same amount of tension spread over a larger area will result in tension per unit area of scar, so in some circumstances it may better to increase the length of the scar in order to better distribute the tension (over a wider surface area). Increasing the length of the scars may also prevent or lessen tissue irregularities in the inferior aspect of the breast.
Breast sensation after breast reduction and breast lift
Breast sensation can change after breast reduction and breast lift. There are typically some temporary changes immediately after surgery, which can include decrease in sensation (termed hypesthesia, most common) and also an increase in sensation (termed hyperesthesia). In one study, approximately 25% of patients getting a breast reduction had some decrease in breast sensation. Because some change in sensation is expected after breast reduction and breast lift, this is more considered an expected consequence than a complication. Many patients that seek breast reduction or breast lift have a decreased level of sensation before surgery. Because of this fact, in order to accurately assess the true change in sensation after breast reduction or breast lift, the sensation must be measured before surgery to allow comparison to sensation after surgery.
Prophylactic antibiotics for breast reduction and breast lift
Patients getting a breast reduction or a breast lift may sometimes develop an infection. In an effort to reduce the infection rate to zero, prophylactic antibiotics may be given before, during, and sometimes after surgery. The most important times to administer antibiotics (if they are administered) are before and during surgery. The literature on the efficacy of antibiotics with breast reduction is mixed (conflicting). Because the incidence of infection is so low with breast reduction and breast lift, it is challenging to collect and analyze data on this problem. For example, a Plastic surgeon may spend an entire career performing breast surgery and during that time see very few patients that develop a breast infection after breast reduction or breast lift. In addition, there are so many factors that may contribute to the patient developing a breast infection that studying one single factor as an isolated cause or prevention is extremely difficult. The indications for use of prophylactic antibiotics may be stronger when a foreign body (for example, mesh or a breast implant) is placed during the procedure. In the event of a breast infection, close follow up and treatment is indicated. If the infection is a cellulitic (diffuse) process, then all that may be required is antibiotics. If the infection is an abscess, then it may require an additional surgical procedure (drainage) and antibiotics.
Combined breast lift and breast augmentation
Some patients may need or desire a breast augmentation in addition to a breast lift. These patients typically present with severe sagging and with a deficiency of breast tissue volume. If both of these procedures are needed or desired, a decision must be made to perform these procedures at the same time, or “stage” the procedures. If the procedures are “staged”, this means that the procedures are performed at different times, with a period in between the procedures. When performing a breast lift (or a breast reduction), in simplest terms, the procedure tightens up the breast. When performing a breast augmentation, in simplest terms, the procedure stretches out the breast. If these two procedures are performed at the same time, the breast lift and the breast augmentation are “fighting each other”, so to speak. The breast lift adversely changes the normal circulation of the breast (interrupts the normal blood supply) as a result of flap development. The breast augmentation also adversely affects the circulation of the breast. Additional pressure on the breast tissues from a breast implant may also decrease the breast circulation. This is especially true if large (oversized) implants are used. If the circulation reaches a critical level (cutting off the circulation), then wound problems may occur including tissue loss, delayed healing, and infection. Some surgeons choose to “stage” these two procedures which allows the blood supply to the breast to reestablish in between the procedures, thereby giving a larger safety factor. Each patient’s situation is different, and the choice to perform these procedures at the same time or to “stage” the procedures is made by the patient after an informed consent process.
Recovery
The recovery after surgery for breast reduction and breast lift is about the same as breast augmentation in most patients. One significant difference between these procedures is the length of the incisions. The incisions in the breast reduction and the breast augmentation are significantly longer in the breast reduction and the breast lift. There is typically some wound drainage after the breast reduction and breast lift procedures as opposed to the breast augmentation where there is little or no drainage. This may result in slightly more postoperative discomfort in the period immediately following surgery. The discomfort for both the breast lift and breast reduction is easily controlled with oral pain medicine in most patients. Because the breast reduction and the breast lift involve the development of tissue flaps, it is very important that the patient avoid cigarettes and other tobacco products before and after breast reduction or breast lift procedures. This includes secondary exposure to tobacco as well. Exposure to these products increases the likelihood of wound complications including infection, tissue loss, and delayed wound healing.
Complications
 As with any surgery, complications can occur with breast reduction and breast lift. Two complications that can occur with any type of surgery are bleeding and infection. Hematoma or bleeding can occur after breast reduction or breast lift surgery, but it is rare (occurs in less than 1% of patients). All wounds have bleeding (inside) after surgery. Of primary importance is whether or not the bleeding is clinically significant. Some patients may be at more risk for bleeding. For example, if a patient has a history of high blood pressure, especially if it is not well controlled, she may be more likely to have bleeding after breast reduction or breast lift surgery. If excess bleeding that is clinically significant does occur, then it may require an additional procedure (exploration and irrigation). In extreme circumstances, which are rare, excessive bleeding may require a blood transfusion. Infection can also occur, and it too is rare (occurs in less than 1% of patients). When infection does occur, it can present as cellulitis or an abscess, both of which are typically treated with antibiotics. In the case of an abscess, a surgical procedure may be needed (exploration, irrigation, and drainage) in addition to antibiotics. Fat necrosis and subsequent calcification can also occur after breast reduction and breast lift. As previously noted, this can make obtaining and interpreting mammograms more challenging. Fat necrosis and calcification can also cause firm areas in the breast, and also cause tenderness in the area of the calcification. Except in the case of the free nipple-areolar complex graft, the nipple-areolar complex is supported (blood supply) by a pedicle (flap). If the blood supply is not adequate to support that tissue, then partial or total loss of the nipple-areolar complex can occur. Partial loss of the nipple-areolar complex is much more common than total loss, but both are very unusual. As with infection and bleeding, some patients are more susceptible to this problem than others, especially patients that use tobacco products (smoke cigarettes). If there is partial loss of the nipple-areolar complex then no extra procedure may be needed. If there is a total loss of the nipple-areolar complex, then a reconstructive procedure may be needed or desired by the patient. Tissue loss can also occur in other areas of the breast. The most susceptible area is at the bottom of the middle of the breast in the inferior pedicle technique, although extensive tissue loss in this area is very rare. Numbness or decreases sensation (hypesthesia) can occur after breast reduction or breast lift. Changes in sensation after surgery are usually not considered a complication but are considered a sequela (it is expected after surgery). In most patients some sensation returns after surgery, but this can take months to occur. Permanent numbness is possible, but this is not common. Hypersensitivity (hyperesthesia) can also occur, but this is less common, and almost always resolves with time. Adverse scarring can occur with any surgical procedure, and can also occur with traumatic wounds. The incision sites are examined frequently immediately after surgery and treated if the need arises. The best predictor of the next scar is the last scar. By examining a patients scars, one can get a general idea if the patient is a “good scar former” or a “bad scar former”. In general, it is reasonable to expect that a patients scar forming ability remain consistent throughout their lifetime which helps in predicting the appearance of future scars (favorable or unfavorable). Unfavorable scars are treated with a variety of modalities. In general, it is much more effective to treat adverse scarring early in its evolution, as opposed to late in its evolution. This emphasizes the importance of regular follow up after surgery, and patients with a history of adverse scarring may be treated preemptively.
As with any surgery, complications can occur with breast reduction and breast lift. Two complications that can occur with any type of surgery are bleeding and infection. Hematoma or bleeding can occur after breast reduction or breast lift surgery, but it is rare (occurs in less than 1% of patients). All wounds have bleeding (inside) after surgery. Of primary importance is whether or not the bleeding is clinically significant. Some patients may be at more risk for bleeding. For example, if a patient has a history of high blood pressure, especially if it is not well controlled, she may be more likely to have bleeding after breast reduction or breast lift surgery. If excess bleeding that is clinically significant does occur, then it may require an additional procedure (exploration and irrigation). In extreme circumstances, which are rare, excessive bleeding may require a blood transfusion. Infection can also occur, and it too is rare (occurs in less than 1% of patients). When infection does occur, it can present as cellulitis or an abscess, both of which are typically treated with antibiotics. In the case of an abscess, a surgical procedure may be needed (exploration, irrigation, and drainage) in addition to antibiotics. Fat necrosis and subsequent calcification can also occur after breast reduction and breast lift. As previously noted, this can make obtaining and interpreting mammograms more challenging. Fat necrosis and calcification can also cause firm areas in the breast, and also cause tenderness in the area of the calcification. Except in the case of the free nipple-areolar complex graft, the nipple-areolar complex is supported (blood supply) by a pedicle (flap). If the blood supply is not adequate to support that tissue, then partial or total loss of the nipple-areolar complex can occur. Partial loss of the nipple-areolar complex is much more common than total loss, but both are very unusual. As with infection and bleeding, some patients are more susceptible to this problem than others, especially patients that use tobacco products (smoke cigarettes). If there is partial loss of the nipple-areolar complex then no extra procedure may be needed. If there is a total loss of the nipple-areolar complex, then a reconstructive procedure may be needed or desired by the patient. Tissue loss can also occur in other areas of the breast. The most susceptible area is at the bottom of the middle of the breast in the inferior pedicle technique, although extensive tissue loss in this area is very rare. Numbness or decreases sensation (hypesthesia) can occur after breast reduction or breast lift. Changes in sensation after surgery are usually not considered a complication but are considered a sequela (it is expected after surgery). In most patients some sensation returns after surgery, but this can take months to occur. Permanent numbness is possible, but this is not common. Hypersensitivity (hyperesthesia) can also occur, but this is less common, and almost always resolves with time. Adverse scarring can occur with any surgical procedure, and can also occur with traumatic wounds. The incision sites are examined frequently immediately after surgery and treated if the need arises. The best predictor of the next scar is the last scar. By examining a patients scars, one can get a general idea if the patient is a “good scar former” or a “bad scar former”. In general, it is reasonable to expect that a patients scar forming ability remain consistent throughout their lifetime which helps in predicting the appearance of future scars (favorable or unfavorable). Unfavorable scars are treated with a variety of modalities. In general, it is much more effective to treat adverse scarring early in its evolution, as opposed to late in its evolution. This emphasizes the importance of regular follow up after surgery, and patients with a history of adverse scarring may be treated preemptively.
 Macromastia is defined as abnormally large breasts. Gigantomastia is defined as extremely large breasts. The quantitative definition of these terms is subjective and more than one definition is acceptable. Macromastia and gigantomastia have been shown to have a negative impact on overall health. The treatment for these problems, termed breast reduction and breast lift (reduction mammaplasty and mastopexy) have been routinely performed for many decades. The primary indications for breast reduction are
Macromastia is defined as abnormally large breasts. Gigantomastia is defined as extremely large breasts. The quantitative definition of these terms is subjective and more than one definition is acceptable. Macromastia and gigantomastia have been shown to have a negative impact on overall health. The treatment for these problems, termed breast reduction and breast lift (reduction mammaplasty and mastopexy) have been routinely performed for many decades. The primary indications for breast reduction are
 As with any surgical procedure, a medical history and physical exam should be performed when considering breast reduction or breast lift, especially for patients that do not receive regular medical care. During the history, information regarding the patient’s general health is assessed. This is especially true for older patients who are more likely to have general health issues (heart, blood pressure) which may complicate the procedure than younger patients. The patient’s symptoms are reviewed (as noted in a previous section) and they fit a typical pattern in most patients. Any psychological or social problems are also reviewed. The patient’s family history related to breast cancer should also be explored. The importance of the patient’s family history of breast cancer becomes more important with advancing age (although it is important at any age) because the incidence of breast cancer increases as age increases. A strong family history of breast cancer should always be considered when planning any type of breast surgery. A family history of breast cancer is a risk for developing breast cancer. In some circumstances, a strong family history of breast cancer may completely change the surgical plan. Some patients have an inherited genetic tendency to develop breast cancer. A percentage of patients have a known genetic trait (BrCa) which increases the risk of breast cancer. If this is suspected, then a consultation with qualified specialist is obtained to complete genetic testing. Fortunately, the minority of patients (based on current data) that develop breast cancer are a result of an identified genetic trait.
As with any surgical procedure, a medical history and physical exam should be performed when considering breast reduction or breast lift, especially for patients that do not receive regular medical care. During the history, information regarding the patient’s general health is assessed. This is especially true for older patients who are more likely to have general health issues (heart, blood pressure) which may complicate the procedure than younger patients. The patient’s symptoms are reviewed (as noted in a previous section) and they fit a typical pattern in most patients. Any psychological or social problems are also reviewed. The patient’s family history related to breast cancer should also be explored. The importance of the patient’s family history of breast cancer becomes more important with advancing age (although it is important at any age) because the incidence of breast cancer increases as age increases. A strong family history of breast cancer should always be considered when planning any type of breast surgery. A family history of breast cancer is a risk for developing breast cancer. In some circumstances, a strong family history of breast cancer may completely change the surgical plan. Some patients have an inherited genetic tendency to develop breast cancer. A percentage of patients have a known genetic trait (BrCa) which increases the risk of breast cancer. If this is suspected, then a consultation with qualified specialist is obtained to complete genetic testing. Fortunately, the minority of patients (based on current data) that develop breast cancer are a result of an identified genetic trait.
 As with any surgery, complications can occur with breast reduction and breast lift. Two complications that can occur with any type of surgery are bleeding and infection. Hematoma or bleeding can occur after breast reduction or breast lift surgery, but it is rare (occurs in less than 1% of patients). All wounds have bleeding (inside) after surgery. Of primary importance is whether or not the bleeding is clinically significant. Some patients may be at more risk for bleeding. For example, if a patient has a history of high blood pressure, especially if it is not well controlled, she may be more likely to have bleeding after breast reduction or breast lift surgery. If excess bleeding that is clinically significant does occur, then it may require an additional procedure (exploration and irrigation). In extreme circumstances, which are rare, excessive bleeding may require a blood transfusion. Infection can also occur, and it too is rare (occurs in less than 1% of patients). When infection does occur, it can present as cellulitis or an abscess, both of which are typically treated with antibiotics. In the case of an abscess, a surgical procedure may be needed (exploration, irrigation, and drainage) in addition to antibiotics. Fat necrosis and subsequent calcification can also occur after breast reduction and breast lift. As previously noted, this can make obtaining and interpreting mammograms more challenging. Fat necrosis and calcification can also cause firm areas in the breast, and also cause tenderness in the area of the calcification. Except in the case of the free nipple-areolar complex graft, the nipple-areolar complex is supported (blood supply) by a pedicle (flap). If the blood supply is not adequate to support that tissue, then partial or total loss of the nipple-areolar complex can occur. Partial loss of the nipple-areolar complex is much more common than total loss, but both are very unusual. As with infection and bleeding, some patients are more susceptible to this problem than others, especially patients that use tobacco products (smoke cigarettes). If there is partial loss of the nipple-areolar complex then no extra procedure may be needed. If there is a total loss of the nipple-areolar complex, then a reconstructive procedure may be needed or desired by the patient. Tissue loss can also occur in other areas of the breast. The most susceptible area is at the bottom of the middle of the breast in the inferior pedicle technique, although extensive tissue loss in this area is very rare. Numbness or decreases sensation (hypesthesia) can occur after breast reduction or breast lift. Changes in sensation after surgery are usually not considered a complication but are considered a sequela (it is expected after surgery). In most patients some sensation returns after surgery, but this can take months to occur. Permanent numbness is possible, but this is not common. Hypersensitivity (hyperesthesia) can also occur, but this is less common, and almost always resolves with time. Adverse scarring can occur with any surgical procedure, and can also occur with traumatic wounds. The incision sites are examined frequently immediately after surgery and treated if the need arises. The best predictor of the next scar is the last scar. By examining a patients scars, one can get a general idea if the patient is a “good scar former” or a “bad scar former”. In general, it is reasonable to expect that a patients scar forming ability remain consistent throughout their lifetime which helps in predicting the appearance of future scars (favorable or unfavorable). Unfavorable scars are treated with a variety of modalities. In general, it is much more effective to treat adverse scarring early in its evolution, as opposed to late in its evolution. This emphasizes the importance of regular follow up after surgery, and patients with a history of adverse scarring may be treated preemptively.
As with any surgery, complications can occur with breast reduction and breast lift. Two complications that can occur with any type of surgery are bleeding and infection. Hematoma or bleeding can occur after breast reduction or breast lift surgery, but it is rare (occurs in less than 1% of patients). All wounds have bleeding (inside) after surgery. Of primary importance is whether or not the bleeding is clinically significant. Some patients may be at more risk for bleeding. For example, if a patient has a history of high blood pressure, especially if it is not well controlled, she may be more likely to have bleeding after breast reduction or breast lift surgery. If excess bleeding that is clinically significant does occur, then it may require an additional procedure (exploration and irrigation). In extreme circumstances, which are rare, excessive bleeding may require a blood transfusion. Infection can also occur, and it too is rare (occurs in less than 1% of patients). When infection does occur, it can present as cellulitis or an abscess, both of which are typically treated with antibiotics. In the case of an abscess, a surgical procedure may be needed (exploration, irrigation, and drainage) in addition to antibiotics. Fat necrosis and subsequent calcification can also occur after breast reduction and breast lift. As previously noted, this can make obtaining and interpreting mammograms more challenging. Fat necrosis and calcification can also cause firm areas in the breast, and also cause tenderness in the area of the calcification. Except in the case of the free nipple-areolar complex graft, the nipple-areolar complex is supported (blood supply) by a pedicle (flap). If the blood supply is not adequate to support that tissue, then partial or total loss of the nipple-areolar complex can occur. Partial loss of the nipple-areolar complex is much more common than total loss, but both are very unusual. As with infection and bleeding, some patients are more susceptible to this problem than others, especially patients that use tobacco products (smoke cigarettes). If there is partial loss of the nipple-areolar complex then no extra procedure may be needed. If there is a total loss of the nipple-areolar complex, then a reconstructive procedure may be needed or desired by the patient. Tissue loss can also occur in other areas of the breast. The most susceptible area is at the bottom of the middle of the breast in the inferior pedicle technique, although extensive tissue loss in this area is very rare. Numbness or decreases sensation (hypesthesia) can occur after breast reduction or breast lift. Changes in sensation after surgery are usually not considered a complication but are considered a sequela (it is expected after surgery). In most patients some sensation returns after surgery, but this can take months to occur. Permanent numbness is possible, but this is not common. Hypersensitivity (hyperesthesia) can also occur, but this is less common, and almost always resolves with time. Adverse scarring can occur with any surgical procedure, and can also occur with traumatic wounds. The incision sites are examined frequently immediately after surgery and treated if the need arises. The best predictor of the next scar is the last scar. By examining a patients scars, one can get a general idea if the patient is a “good scar former” or a “bad scar former”. In general, it is reasonable to expect that a patients scar forming ability remain consistent throughout their lifetime which helps in predicting the appearance of future scars (favorable or unfavorable). Unfavorable scars are treated with a variety of modalities. In general, it is much more effective to treat adverse scarring early in its evolution, as opposed to late in its evolution. This emphasizes the importance of regular follow up after surgery, and patients with a history of adverse scarring may be treated preemptively.